By Stephanie Gadlin, Special to the Crusader/Inland Foundation Fellow
The cardiac arrest of Buffalo Bills safety DeMar Hamlin during a nationally televised football game sent shockwaves across the country. The incident sparked renewed interests in cardiovascular health among African Americans as well as a closer look at the role the coronavirus pandemic and race has played in its rise.
Hamlin, 24, had just made a tackle in a January 2nd game against the Cincinnati Bengals when he collapsed mid-play. As his teammates wept and prayed and a televised audience watched in real-time, Hamlin’s heartbeat was restored on the field by medics before he was transferred to a hospital in critical condition where he eventually recovered. Since then, the pro athlete has become the poster child of heart health and he recently launched a campaign to promote cardiopulmonary resuscitation (CPR) as essential to lifesaving.
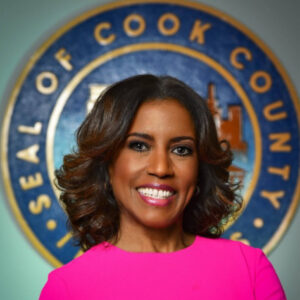
Last week, Cook County Commissioner Donna Miller (6th District) introduced a resolution making it a fiscal priority to promote efforts to address heart disease, which is the leading cause of death in Cook County. In 2019, she also developed a countywide CPR training program that has led to hundreds of county employees becoming skilled in CPR. The south suburban leader said, “Education and training efforts are crucial to improving health outcomes for those who experience cardiac distress, and I’m proud that our office is playing a part in keeping our residents safe and healthy.”
Hamlin is only one of many recent health scares and/or incidents deaths involving seemingly healthy young adults, under age 40, and teens, from heart-related issues. According to the American College of Cardiology, the percentage of young people having a heart attack has been increasing by 2 percent each year for the last 10 years, with COVID-19 leaving a substantial impact on that very demographic.
“This occurs across the spectrum of patients, even young people. So, the greatest per capita increase in heart attacks and strokes that we’ve seen have been in the 30- and 40-year old’s,” said Dr. Lon Young, chief medical officer of CapRock Health systems in Ohio. “And it is worse after having COVID because it causes inflammation of blood vessels which can lead to problems like heart attack and stroke.”
Additional research shows patients with COVID-19 were at increased risk of a broad range of cardiovascular disorders including cerebrovascular disorders, dysrhythmias, ischemic and non-ischemic heart disease, pericarditis, myocarditis, heart failure, and thromboembolic disease. The risk of heart failure increased by 72 percent, or around 12 more people in a COVID-19 study group per 1,000 studied. Hospitalization increased the likelihood of future cardiovascular complications, but even people who avoided hospitalization were at higher risk for many conditions.
A study published last year by Nature Medicine found that in the year after recovering from the illness’s acute phase, patients had increased risks of an array of cardiovascular problems, including abnormal heart rhythms, heart muscle inflammation, blood clots, strokes, myocardial infarction, and heart failure, including among those who weren’t hospitalized with acute COVID-19.
Prior to the pandemic, African Americans were still most likely to suffer and die from cardiovascular disease (CVD). According to the Center for Disease Control (CDC), 697,000 people (or 1-in-5) in the U.S. deaths in 2020 were the result of heart disease. In Illinois, 26,282 deaths were due to the result of heart disease in 2021. African Americans represent almost 21 percent of all deaths in Illinois in that year.
The most recent death CDC data suggests that among non-Hispanic Black adults 20 years of age and older, 60.1 percent of males and 58.8 percent of females had CVD. In 2019, heart disease caused the deaths of 57,761 Black males and 54,544 Black females. Since 2020, more than one million people have died as a result of COVID-19—13.9 percent of which were Black.
The data suggests people who had recovered from COVID-19 showed stark increases in 20 cardiovascular problems over the year after infection. For example, they were 52 percent more likely to have had a stroke than the contemporary control group, meaning that, out of every 1,000 people studied, there were around 4 more people in the COVID-19 group than in the control group who experienced stroke.
Black people in the United States have the worst health and worst health outcomes across the board, according to numerous research reports and data. Cancer, heart disease, diabetes, homicides are exacerbated by many social detriments such as lack of transportation, unemployment, and food insecurity.
Heart attacks occur when a coronary artery leading to the heart is blocked, which prevents blood from reaching the organ. A “cardiac arrest” essentially is the cessation of heart activity or a stopping of the heart pumping, which is generally due to what’s called an arrhythmia or an electrical disturbance of the heart. A stroke occurs when the blood supply to part of the brain is interrupted or reduced, preventing brain tissue from getting oxygen and nutrients, according to the Mayo Clinic.
The AHA says, heart disease cost the U.S. about $229 billion each year and includes the cost of health care services, medicines, and lost productivity due to death. The numbers also show more than 350,000 cardiac arrests occurring outside of a hospital.
In addition to the traditional factors of obesity, high blood pressure, inactivity, unhealthy diets and drug and alcohol abuse, the AHA found that structural racism was a contributing factor as well. To address the disparity, two years ago the global organization committed to raise more than $230 million to address the barrier to achieving equitable health. In collaboration with the U.S. department of health it also launched a $121 million nationwide high blood pressure initiative focused primarily on health outcomes among racial and ethnic minority populations.
Another challenge emerged post pandemic via the exodus of professionals working in the health care, which has left many local hospital and neighborhood clinics understaffed and under resourced on both the administrative and medical services side, especially in under-served, low-income neighborhoods.
The AHA pledge $100 million more to address targeted, community-level health equity barriers through its Social Impact Fund, the Bernard J. Tyson Social Impact Fund, as well as its community-based issues campaigns, including those of its Voices for Healthy Kids initiative. In Chicago, organizations such as 40 Acres Fresh Market and Sweet Potato Patch, received funds to advance heart health education and remove barriers to access to healthcare.

AHA National Vice President of Health and Equity Partnerships Pamela Gorman Johnson spoke to the Crusader about the program, “We are also investing in community-based solutions meaning we are providing grants and capital to social enterprises that are addressing the social determinants of health,” she said. “In order to meet people where they are, we need solutions that actually meet people where they are and with a trusted voice.”
Johnson, who also serves as executive director of the National Hypertension Control Initiative, also said health education matters, “What we have created is an eco-system that utilizes the platform called ‘Unite Us’ which has community and faith-based organizations on a singular platform,” she said. “We are putting the infrastructure in place. We’ve got to start connecting the dots for the individual that’s why it is critical that we invest in hyper local, community-led solutions to address health inequity and addressing those basic needs that can lead to create barriers.”
Reporting made possible by the Inland Foundation






